 During her career, Dr. Ratajczak developed an ELISA assay for Rat Alpha-2-Macroglobulin, the most sensitive acute phase reactant protein for the rat, and also quantitated acute phase reactant proteins in the dog and monkey. She also conducted acute toxicology studies and both in vivo and in vitro immune assays, and has studied the immunotoxicologic properties of many compounds, including immunosuppressive and immunostimulatory drugs, in several animal species including mice, rats, nonhuman primates, and humans.
During her career, Dr. Ratajczak developed an ELISA assay for Rat Alpha-2-Macroglobulin, the most sensitive acute phase reactant protein for the rat, and also quantitated acute phase reactant proteins in the dog and monkey. She also conducted acute toxicology studies and both in vivo and in vitro immune assays, and has studied the immunotoxicologic properties of many compounds, including immunosuppressive and immunostimulatory drugs, in several animal species including mice, rats, nonhuman primates, and humans.
We continue on with my interview.
Q. 10. Will you please contrast a single dose vaccine versus multiple dose vaccines.
In the past, many vaccines were packaged in large vials so that multiple doses could be given from the same vial. These vials typically contained thimerosal to inhibit the growth of bacteria that might be introduced as a result of entering the vial multiple times. In contrast, a single dose vaccine is one that is packaged in a vial containing only one dose. Thus the vial is only entered a single time, and typically does not contain any anti-bacterial agents.
Q. 11. Can you talk about ‘hidden’ vaccine adjuvants that do not appear on package inserts, e.g., peanut oil in particular, and any impact that it may have had on so many children having peanut allergies now.
In the 1968 Hong Kong influenza pandemic, a new vaccine preparation was tested. In a publication in 1969, it is stated an influenza vaccine in adjuvant 65 (made with peanut oil) increased the antibody response to influenza virus even when the antigen was reduced 4-fold or more. In addition, the use of the adjuvant gives a considerable broadening of antibody response against diverse serotypes. At the time of publication, the authors state the vaccine in adjuvant 65 had been given to more than 16000 persons without untoward effect. In addition, no pyrogenic or other systemic reaction has been noted to follow vaccine in adjuvant 65, in contrast to the reaction which sometimes follows aqueous vaccine (Hilleman, 1969). Other investigators confirm the advantages of the use of adjuvant 65 in the influenza vaccine, with an increase in antibody titer and a broader response to both Influenza A and B antigens. Subjective reactions each of 5 days following vaccination showed more pain was recorded by recipients of the oil adjuvant compared with those given an aqueous preparation, but local redness was more frequent after the aqueous vaccine, and systemic symptoms were recorded a little more often after aqueous than oil adjuvant vaccine (Smith et al., 1975). However, no mention was made of looking for reactions to other components of the vaccine, such as the peanut antigen. When a vaccine is given, an immune response follows. This response can be specific for any of the components of the vaccine, including the source of oil in the adjuvant. In this case, that would be the peanut. Therefore, a vaccine containing peanut oil could cause allergy to the peanut. The “inactive” components of the vaccine need not be listed on the ingredients list (Gregory, 2009). [CJF emphasis]
Q. 12. Please talk about how adjuvants are designed to over-stimulate immune response that, in turn, can attack brain microglia and astrocytes. What happens? Do adjuvants interfere with nerve pathway development? Do they incite glutamate and quinolenic acid? What are the resultant consequences?
The adjuvant and the antigen are two separate components of a vaccine. The antigen is the component that the vaccine is designed to protect against, such as influenza. The adjuvant is the added component that causes an enhancement of the immune response by slowing the release of the antigen into the body. The immune system responds to the presence of antigen and terminates the response once the antigen is eliminated. When the antigen is mixed with an insoluble adjuvant, a focus is formed, and the antigen within the focus slowly leaks into the body, giving a prolonged antigenic stimulus. (Tizard, 1988).
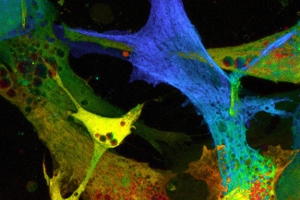
In the case of the immune system’s attack on brain microglia and astrocytes, there is a cross reaction of the antibody against the antigen and the brain cells. (The configuration of the brain cells or parts of them is similar to the antigen.) Therefore, the immune system attacks the brain cells. [Refer to HVR’s answer to question 1 in Part 1.]
The adjuvant, as stated above, causes the antigen to be released to the body very slowly, thus augmenting the immune response. Indirectly, the adjuvant could be responsible for the interference with the development of nerve pathways, but the direct reason is the cross-reaction of specificity of the immune system.
Besides eliciting an immune response that is specifically against the antigen, the vaccine elicits a number of cytokines or factors, which enhance or regulate the immune response. The cytokines caused by the vaccine cause the secretion of harmful chemicals including two excitotoxins, glutamate and quinolenic acid (Blaylock, 2008). These chemicals elicit an excitatory reaction in the neurons, and create cellular toxicity and inflammation if too much accumulates (Jepson, 2007; Reynolds, 2007).
Q. 13. Please talk about aluminum adjuvants, which come in four formulations. Is any one more harmful than the others? Aluminum hydroxide, aluminum hydroxyphosphate sulfate, aluminum phosphate, aluminum potassium sulfate.
The aluminum adjuvants are effective in increasing the immunogenicity of vaccines. The four adjuvants listed are currently used in childhood vaccines such as DTaP, Hep A, Hep B, HiB, human papillomavirus (HPV), DTaP, DTAP-HepB-IPV, Pneumococcal DT, Td, etc. These four adjuvants have different isoelectric points and properties, and they are not interchangeable. The efficacy of each salt as an adjuvant depends also on the characteristics of the antigens in the vaccine. Adverse reactions include sterile abscesses, erythema, subcutaneous nodules, granulomatous inflammation and contact hypersensitivity (Eickoff and Myers, 2002.) I have not found data on the relative toxicity of these four aluminum adjuvants. However, in the workshop summary on aluminum in vaccines, Eickhoff and Myers report that Aventis Pasteur, France has planned studies and is already working on examination of the evolution of aluminum adjuvant-associated histology. In addition, in vitro studies of human macrophages exposed to various aluminum salts are planned.
Aluminum-containing vaccines have more than a 75-year record of safety around the world, with serious adverse effects being rare. (National Network for Immunization Information, 2008). Despite this, many manifestations of the toxicity of aluminum are documented.
Aluminum is established as a neurotoxin, although the basis for its toxicity is unknown. Aluminum alters the function of the blood-brain barrier, which regulates exchanges between the central nervous system and peripheral circulation. Aluminum increases the rate of transmembrane diffusion and selectively changes saturable transport systems without disrupting the integrity of the membranes or altering central nervous system hemodynamics. Such alterations in the access to the brain of nutrients, hormones, toxins, and drugs could be the basis of central nervous system dysfunction. (See Banks and Kastin, 1989).
Aluminum in vaccines has a potential to induce serious immunological disorders in humans, particularly autoimmunity, long-term brain inflammation and associated neurological complications. (See Tomljenovic and Shaw, 2011).
Macrophagic myofascitis is a term used to describe microscopic findings in some muscle biopsies. The lesions are thought to be caused by tissue changes resulting from the normal immune response to the aluminum-absorbed vaccine (Verdier, 2005). In France, biopsy findings are described in adult patients who had muscle and joint aches and pains and fatigue. The physician who first described the biopsy findings proposed that aluminum-containing vaccines caused the symptoms (Gherardi, 1998).
In another report, aluminum hydroxide injections are tied to motor deficits and motor neuron degeneration (Shaw and Petrick, 2009).
Q. 14. Can you please discuss the interaction of mercury as found in Thimerosal (49.6% Hg) and aluminum together in a vaccine.
The addition of Thimerosal to a vaccine in an adjuvant containing aluminum can result in a synergistic toxicity. (See Haley, 2005). Haley reports that aluminum hydroxide alone showed no significant death of neuron cells in culture at six hours, and only slight toxicity over 24 hours. Similarly, Thimerosal caused only a slight increase in neuron death at 6 hours. When Thimerosal and aluminum hydroxide were added together, neuronal death increased to 60%. This is an example of a synergistic effect of two toxicants. [CJF emphasis]
Continued in Part 3
References listed at the end of Part 3.
